Intestinal inflammation can impair mucosal healing, thereby establishing a vicious cycle leading to chronic inflammatory bowel disease (IBD). However, the signaling networks driving chronic inflammation remain unclear. Here we report that CD4+ T cells isolated from patients with IBD produce high levels of interleukin-22 binding protein (IL-22BP), the endogenous inhibitor of the tissue-protective cytokine IL-22. Using mouse models, we demonstrate that IBD development requires T cell–derived IL-22BP. Lastly, intestinal CD4+ T cells isolated from IBD patients responsive to treatment with antibodies against tumor necrosis factor–a (anti–TNF-a), the most effective known IBD therapy, exhibited reduced amounts of IL-22BP expression but still expressed IL-22. Our findings suggest that anti–TNF-a therapy may act at least in part by suppressing IL-22BP and point toward a more specific potential therapy for IBD.
Pelczar P, Witkowski M, Perez LG, et al. Science. 2016;354(6310):358-362.
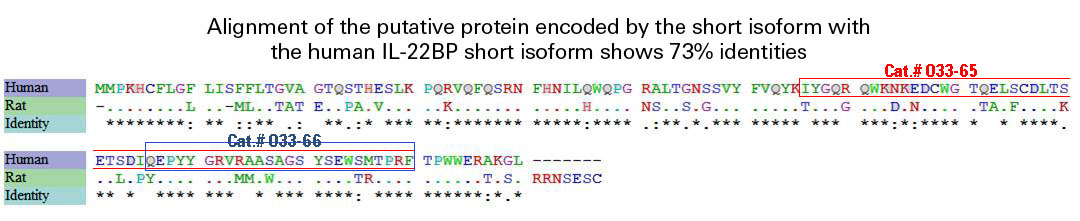
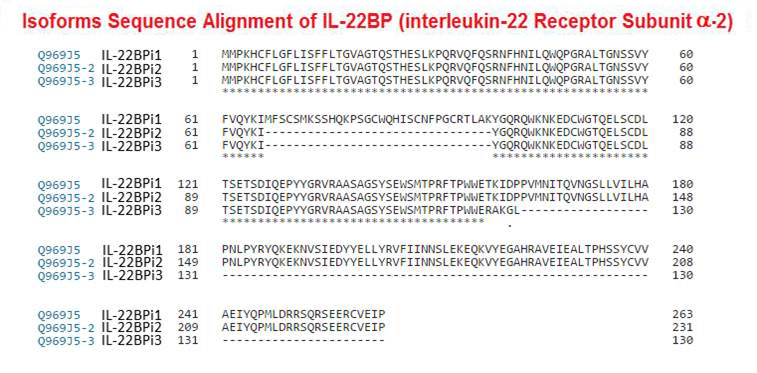
The cytokine interleukin-22 (IL-22), which is a member of the IL-10 family, is produced exclusively by immune cells and activates signal transducer and activator of transcription 3 (STAT3) in nonimmune cells, such as hepatocytes, keratinocytes, and colonic epithelial cells, to drive various processes central to tissue homeostasis and immunosurveillance. Dysregulation of IL-22 signaling causes inflammatory diseases. IL-22 binding protein (IL-22BP; encoded by IL22RA2) is a soluble IL-22 receptor, which antagonizes IL-22activity and has genetic associations with autoimmune diseases. Humans have three IL-22BP isoforms, IL-22BPi1 to IL-22BPi3, which are generated by alternative splicing; mice only have an IL-22BPi2 homolog. We showed that, although IL-22BPi3 had less inhibitory activity than IL-22BPi2, IL-22BPi3 was more abundant in various human tissues under homeostatic conditions. IL-22BPi2 was more effective than IL-22BPi3 at blocking the contribution of IL-22 to cooperative gene induction with the inflammatory cytokine IL-17, which is often present with IL-22 in autoimmune settings. In addition, we found that IL-22BPi1 was not secreted and therefore failed to antagonize IL-22 signaling. Furthermore, IL-22BPi2 was the only isoform that was increased in abundance when myeloid cells were activated by Toll-like receptor 2 signaling or retinoic acid, a maturation factor for myeloid cells. These data suggest that the human IL-22BP isoforms have distinct spatial and temporal roles and coordinately fine-tune IL-22-dependent STAT3 responses in tissues as a type of rheostat.
Lim C, Hong M, Savan R. Sci Signal. 2016;9(447):ra95.
C-X-C motif chemokine receptor type 2 (CXCR2), a key regulatory protein, has been associated with multiple roles in the progression of numerous tumors, including gastric adenocarcinoma (GA). However, the mechanism of CXCR2 in the development of tumors remains controversial and unclear. In a previous study, the expression of CXCR2 and interleukin-22 receptor 2 (IL-22BP) was observed in GA. This promoted the present study, which aimed to explore the association between the two proteins, and to further analyze their roles in GA. CXCR2 and IL-22BP protein expression was analyzed by immunohistochemistry and reverse transcription-quantitative polymerase chain reaction assays in gastric cancer (GC) tissue, additionally confirmed via western blotting and immunocytochemical analysis in the MKN-45, BGC-823 and SGC-7901 cell lines. The association between expression levels and clinicopathological characteristics was evaluated by the Mann-Whitney U and Kruskal-Wallis tests. Using Kaplan-Meier plots and Cox proportional hazard models, overall survival (OS) was analyzed. Compared with non-cancerous tissue, CXCR2 and IL-22BP were over expressed (P<0.001 and P<0.001, respectively), and were observed mainly in the cytoplasm (P=0.022 and P=0.014, respectively) in GA. The associated protein and messenger RNA levels were analyzed, and coexpression was identified. Increased expression and more positive cases of CXCR2 and IL-22BP were observed with advanced pathological tumor-node-metastasis (p-TNM) stage in GC (P<0.001 and P<0.001, respectively), as well as the presence and absence of lymph node metastasis (LNM) (P=0.003 and P=0.041, respectively) and deep or superficial muscular invasion (P=0.002 and P=0.004, respectively). In addition, an association between IL-22BP and tumor diameter was indicated (P=0.021). In a Kaplan-Meier analysis, compared with negative expression, the two proteins identified a group of patients with the shortest OS. Cox proportional hazard models revealed that the two proteins, in addition to p-TNM stage, LNM and depth of invasion, predicted a short time to OS. The coexpression of CXCR2 and IL-22BP was demonstrated in GA, which may indicate that CXCR2 is involved in more complex mechanisms and roles, and indicate a poor outcome in GA progression.
Yang SB, Han F, Wu JH, Zhao Z, Zhan W. Oncol Lett. 2016;12(2):1477-1484.
Interleukin (IL)-22 acts on epithelia, hepatocytes, and pancreatic cells and stimulates innate immunity, tissue protection, and repair. IL-22 may also cause inflammation and abnormal cell proliferation. The binding of IL-22 to its receptor is competed by IL-22 binding protein (IL-22BP), which may limit the deleterious effects of IL-22. The role of IL-22 and IL-22BP in chronic liver diseases is unknown. We addressed this question in individuals chronically infected with schistosomes or hepatitis C virus (HCV). We first demonstrate that schistosome eggs stimulate production of IL-22 transcripts and inhibit accumulation of IL22-BP transcripts in schistosome-infected mice, and that schistosome eggs selectively stimulate production of IL-22 in cultures of blood leukocytes from individuals chronically infected with Schistosoma japonicum. High IL-22 levels in cultures correlated with protection against hepatic fibrosis and portal hypertension. To test further the implication of IL-22/IL-22BP in hepatic disease, we analyzed common genetic variants of IL22RA2, which encodes IL-22BP, and found that the genotypes, AA, GG of rs6570136 (P=0.003; odds ratio [OR]=2), and CC, TT of rs2064501 (P=0.01; OR=2), were associated with severe fibrosis in Chinese infected with S. japonicum. We confirmed this result in Sudanese (rs6570136 GG [P=0.0007; OR=8.2], rs2064501 TT [P=0.02; OR=3.1]), and Brazilians (rs6570136 GG [P=0.003; OR=26], rs2064501 TC, TT (P=0.03; OR=11]) infected with S. mansoni. The aggravating genotypes were associated with high IL22RA2 transcripts levels. Furthermore, these same variants were also associated with HCV-induced fibrosis and cirrhosis (rs6570136 GG, GA [P=0.007; OR=1.7], rs2064501 TT, TC (P=0.004; OR=2.4]). CONCLUSIONS: These results provide strong evidence that IL-22 protects against and IL-22BP aggravates liver fibrosis and cirrhosis in humans with chronic liver infections. Thus, pharmacological modulation of IL-22 BP may be an effective strategy to limit cirrhosis.
Sertorio M, Hou X, Carmo RF, et al. 2015;61(4):1321-31.
Expression of IL-22 is induced in several human inflammatory conditions, including inflammatory bowel disease (IBD). Expression of the IL-22 receptor is restricted to innate immune cells; however, the role of IL-22 in colitis has not yet been defined. We developed what we believe to be a novel microinjection-based local gene-delivery system thatis capable oftargeting the inflamed intestine. Using this approach, we demonstrated a therapeutic potency for IL-22–mediated activation of the innate immune pathway in a mouse model of Th2- mediated colitis that induces disease with characteristics similar to that of IBD ulcerative colitis (UC). IL-22 gene delivery enhanced STAT3 activation specifically within colonic epithelial cells and induced both STAT3- dependent expression of mucus-associated molecules and restitution of mucus-producing goblet cells.Importantly, IL-22 gene delivery led to rapid amelioration of local intestinal inflammation. The amelioration of disease by IL-22 was mediated by enhanced mucus production. In addition, local gene delivery was used to inhibit IL-22 activity through overexpression of IL-22–binding protein. Treatment with IL-22–binding protein suppressed goblet cell restitution during the recovery phase of a dextran sulfate sodium–induced model of acute colitis. These data demonstrate what we believe to be a novel function for IL-22 in the intestine and suggest the potency of a local IL-22 gene–delivery system for treating UC.
| Catalog# | Product | Standard Size | Price |
|---|---|---|---|
| 036-01 | Interleukin-1 (IL-1) (163-171), beta (Human) | 1 mg | $69 |
| 036-08 | Interleukin-1 (IL-1) (165-181), beta (Rat) | 200 µg | $97 |
| 036-02 | Interleukin-1 (IL-1) (193-195), beta analog | 5 mg | $108 |
| 036-05 | Interleukin-2 (IL-2) (126-138) / T-Cell Growth Factor (126-138) (Human) | 200 µg | $69 |
| 036-03 | Interleukin-2 (IL-2) (44-56) / T-Cell Growth Factor (44-56) (Human) | 200 µg | $69 |
| 036-04 | Interleukin-2 (IL-2) (60-70) / T-Cell Growth Factor (60-70) (Human) | 200 µg | $69 |
| 036-06 | Interleukin-2 (IL-2) Receptor Protein (1-11) | 200 µg | $69 |
| 036-07 | Interleukin-2 (IL-2) Receptor Protein (139-145) | 200 µg | $55 |
Social Network Confirmation